Do you have COVID-19? We can help.
There are 3 main types of testing: Diagnostic (identifying current infection), Screening (identifying potentially contagious but asymptomatic individuals), and Surveillance (identifying community-level infection).
We will focus on diagnostic testing, i.e. conducting tests to identify current infection in:
- A symptomatic individual with signs or symptoms that may be consistent with COVID-19, or
- An asymptomatic individuals with recent known or suspected exposure to SARS-CoV-2.
There are 2 main methods. So which one is best? Well, it depends.
Testing methods
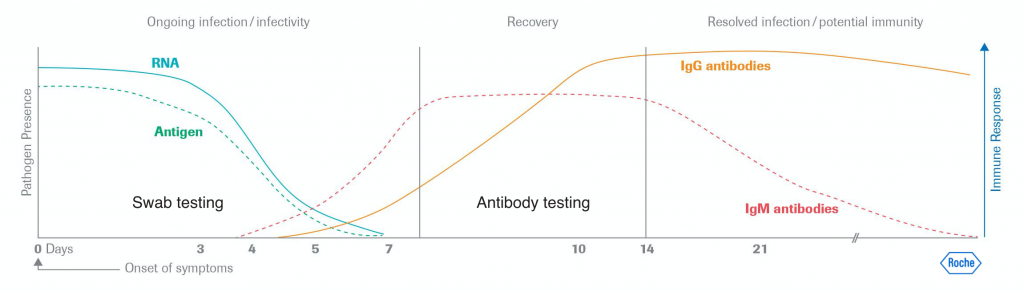
Reference Lab Molecular test
- Method
- What it detects
Viral RNA in nose or throat swabs
- How accurate
About 95%
- Use and Timeframe
3 days after exposure, and
No later than 7 days since onset of symptoms - PRO
Accuracy
- CON
24-hour wait or longer for results (when sent to reference labs)
- Verdict
The Reference Standard
AccessBio Antigen Test
- Method
- What it detects
Viral antigen (a part of the virus) in nasal swabs
- How accurate
About 88%
- Use and Timeframe
3 days after exposure, and
No later than 5 days since onset of symptoms - PRO
Speed: result within 10 minutes
- CON
Negative result requires molecular confirmation
- Verdict
Useful in quickly identify infectious cases
So what does that all mean anyway, all these jargons? Let us look at the picture below.
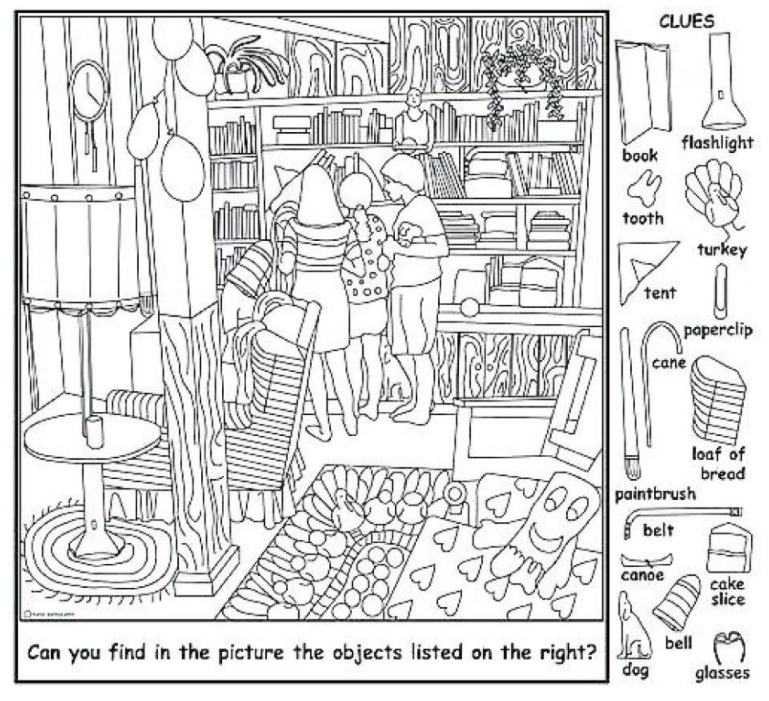
Can you find at least one heart? Well, that is so easy, you will say. They are just right there on the picture, and there are several of them grouped close together, so at least one of them can be easily spotted by you. And that is what RT-PCR will do for you: the process creates multiple copies of the same, so the task is much easier.
Now try looking for the paper clip. Can you find it?
- If you say, “No, I could not find it, and am sure it is not there“, that is an equivalent of a false negative — saying something is not there when it is actually is.
- So after a minute or two, you found it. It was not easy, but you did it. That is what it is like running an antigen test too early in the course of illness. There is only 1 or 2 copies, and it is not so easily found, if at all.
- Supposedly now a few more paper clips were strategically placed in the picture, with some of them easier to be found than others, you will likely find all of them pretty easily. That is what it is like running an antigen test later on in the illness.
So the best case scenario is to get a rapid antigen test is at least 3 days after exposure (to allow for more copies of the virus to be present), and no later than 5 days after onset of symptoms (antigen levels fading significant after day 5). If the likelihood of infection is high but the antigen test is negative (falsely, in this case), then a RT-PCR molecular confirmation test is needed.
The likelihood of infection is highest when:
- There was recent exposure to a person with confirmed COVID-19,
- The individuals have symptoms indicating COVID-19 is likely, and/or
- Diagnostic tests for other causes are negative.
Regarding the Access Bio antigen test, the specificity is very high, approaching 100%, so a false positive rate is very unlikely.
The false negative rate, such as when an infectious person wrongly tested negative, is about 12%, hence the need to confirm with molecular tests when the likelihood of infection is high. Without such confirmation test, the individual should be presumed to be positive for SARS-CoV-2 infection.
Need to get tested?
Open to Established and New patients






